Bacteria can shapeshift to avoid detection and resist antibiotics, a study published in Nature Communications has found. This discovery could unlock a method of combating at least one type of antibiotic resistance—a phenomenon the World Health Organization lists as one of the greatest threats to public health and security.
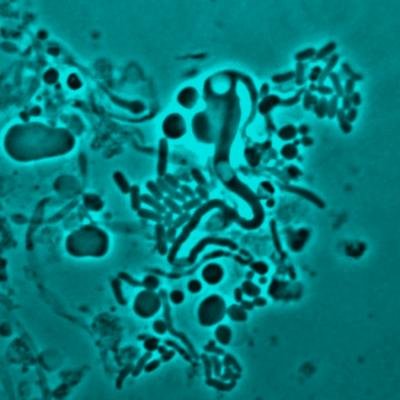
According to the authors of the report, this is the first time bacteria have been shown to change their form inside the human body. They do so dropping their cell wall (a process called L-form switching)—the primary target of several classes of antibiotics. This enables germs to go under the radar, and avoid being picked up by drugs, although it can leave them more vulnerable to the human immune system.
Lead author Katarzyna Mickiewicz, a researcher at the U.K.'s Newcastle University, compares the cell wall to a high-vis jacket.
"This gives them a regular shape (for example a rod or a sphere), making them strong and protecting them but also makes them highly visible—particularly to human immune system and antibiotics like penicillin," she explained.
"What we have seen is that in the presence of antibiotics, the bacteria are able to change from a highly regular walled form to a completely random, cell wall-deficient L-form state—in effect, shedding the yellow jacket and hiding it inside themselves."
The human body can not easily recognize the camouflaged bacteria, and neither can antibiotics.
Mickiewicz and her team came to this conclusion after analyzing samples taken from elderly patients suffering from recurring urinary tract infections (UTIs). Twenty-nine of the 30 samples analyzed contained bacteria that had changed shape—though the precise strain of bacteria varied. L-forms E. coli, Enterococcus, Enterobacter and Staphylococcus were detected.
Previous research has shown that L-form switching can be triggered by the immune system, but it is antibiotic treatment that seems to be the more common cause. The researchers were also able to show that the process can take place in the context of a whole living organism (a zebrafish) and not just in a lab setting.
Mickiewicz told Newsweek she believes L-switching takes place all the time but the lack of cell wall makes the bacteria more fragile and, therefore, more likely to be cleared by an immune attack. However, in those who are immuno-compromised from age or a health-related condition like HIV, enough can survive to create a problem and cause another infection.
"More research is needed to look for L-forms in patients because they are not picked up by normal hospital lab practices," she said.
"It is possible that L-form switching might be relevant not only for UTI but also for many other types of recurrent infection, including sepsis and lung infections."
The good news: "The solution could be straightforward: to combine the usual antibiotics with drugs that kill L-forms."
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.





