WHEN HE REGAINED consciousness last Monday, Jan. 25, Matthew Scott had the uncanny sensation that he had been there before. He was in a busy operating room, the staff swirling around him, his left arm swathed in a pile of white bandages. ""I flashed back to when I lost my hand 13 years ago,'' Scott, 37, told NEWSWEEK. It was all so familiar: ""the feeling of coming out of anesthesia, the odd feeling of discomfort in my arm, the "Oh, Matt, are you OK?' questions.'' But when he woke up this time, he knew things were profoundly different. As he described the experience during an exclusive interview in his room at Jewish Hospital in Louisville, Ky., last Thursday, the tips of five fingers, barely visible, protruded from the billow of gauze. ""I wasn't injured and with a loss,'' he said. ""I was gifted and something was replaced.''
Last week Scott became the first American, and only the third person anywhere, to receive a hand transplant from another person. The operation took nearly 15 hours and involved more than 51 surgeons, nurses and researchers--the experimental edge of microsurgery and human body-shop technology. Jewish Hospital, which pioneered research on the transplant, donated all hospital costs; the doctors worked without compensation. The operation, as Scott knows, carries risks that cannot be assessed yet. His immune system may still reject the hand, forcing surgeons to re-amputate. Or the drugs used to prevent this may shorten his life. Even if it is successful, Scott can only hope to regain partial use of the hand. And like many new medical breakthroughs, the transplant raises ethics questions that the technology cannot address: should doctors use potentially deadly remedies when a patient's life is not at risk?
Already last week the story took a macabre twist. Though the hand donor was supposed to be anonymous, even to Scott, tabloid snooping pressed the man's family to reveal his identity: Glenn William Johnson, a convicted murderer who took his own life the day prior to the operation. In a statement issued by the hospital, Scott offered sympathy first for Johnson's family and gratitude for ""the wonderful gift of my new left hand. While the other aspects of my donor's life seem to be the focus of massive media attention, his precious gift of life . . . can never be overshadowed.''
The operation caps a long ordeal in Scott's life. Just before Christmas 1985, he was lighting an M-80 firework with a cigarette when the fuse skipped faster than he anticipated. The blast tore through his left, dominant, hand, severing tissues, veins and nerves in its path. Scott was a paramedic, familiar with the sight of catastrophic injury, but this was bad. Doctors in New Jersey amputated the hand just above the wrist, replacing it with a prosthetic limb that could open and close, but little more. The prosthesis allowed him to continue his work, but ""he just never felt whole,'' says his mother, Mary Lou Scott. Some nights he paced the halls, unable to sleep for the ""phantom pain'' where his hand used to be. More than anything, he desired a real hand again. When he read a newspaper story about the Jewish Hospital team last summer, he hoped the anguish and self-recrimination were over.
In his hospital room last week, as a guard stood watch against media intruders, Scott weighed the risks of his operation against the benefits. How many years of his life would he be willing to sacrifice for a new hand? He twisted uncomfortably. ""I don't know--is five years too much?'' As his wife, Dawn, nursed a can of diet soda, Scott spoke cogently and thoughtfully despite his pain medication, pausing to answer his own question. ""Well, sure,'' he said. ""With the life that I have, the wife that I have and the children that I have, [five years] is certainly too much. My doctors and I will make that decision when the risks are becoming more than I can handle. If they say, "Matthew, you're going to lose five years of your life, what are you going to do?' I don't know. I'll have to answer that when it comes up.''
By the sometimes dizzying standards of modern medicine, the surgical procedure was complex but unexceptional, a matter of high-tech snipping and sewing (below). Surgeons have been able to reattach patients' own severed hands, with some degree of success, since the 1960s. But for Scott, the tricky part is yet to come. Human immune systems are designed to attack any foreign organic matter entering the body. To prevent such an assault against his new hand, Scott must take a powerful cocktail of drugs to suppress his immune system, leaving him defenseless against diseases and infections. The protocol runs about $15,000 per year, and calls for him to take more than 10 pills throughout each day. Even with the drugs, says Dr. Warren Breidenbach, who led the transplant team, the odds of his body's completely rejecting the hand in the first year are about 50-50. If this happens, doctors will be forced to re-amputate.
The drugs also have toxic side effects, which can include kidney damage, cataracts, ulcers and a cancer of the lymph glands called post-transplant lymphoproliferative disorder, or PTLD. ""It can kill you,'' says Breidenbach. After the initial course, Breidenbach hopes to phase out the most toxic drug. However, he acknowledges, ""Even if you stop the immunosuppression, lymphoma can go on and kill the patient. That's what we're most worried about.'' Scott is also taking an anti-inflammatory called Prednisone, which can damage the pancreas and lead to diabetes--a particular worry because Scott is already diabetic.
In the last few decades, doctors have made remarkable strides in transplanting vital organs. But the hand poses special difficulties: Scott's immune system must accept ""composite tissues'' made up of nerves, tendons, muscles, skin, bones and bone marrow. His own skin will likely be the most aggressive against the new tissue. As our body's natural armor, skin fends off pathogens like bacteria and viruses. ""That's why we're able to live,'' says Dr. Neil Jones, chief of hand surgery at the UCLA Medical Center. ""That's why human life has evolved.''
Scott is under counsel not to move his fingers, for fear of tearing the stitches holding together the tendons. But last Tuesday, he was able to wiggle the index finger--a boost for his morale, says Breidenbach, more than a diagnostic test. ""We knew he couldn't help himself.'' Scott cannot yet feel his new hand. ""What I do feel is a very general feeling of discomfort, nothing local. No one's sure about the physiology behind it . . . Is it that the nerves are starting to regenerate and now my mind is remembering? Is it the last known feeling I had and I'm reverting back to that? Or is it because the nerve endings have been stitched together and some sensation is now going through? We can't know until things start to progress.''
In September, four months before Scott's operation, an international team of doctors in Lyon, France, performed a groundbreaking transplant on a man named Clint Hallam, who lost his hand in a circular-saw accident while serving two years in a New Zealand prison for fraud. (The only previous attempt, undertaken in 1964, had failed after just two weeks.) Between the eighth and ninth week after surgery, Hallam's skin developed red, inflamed lesions resembling eczema, signs that his skin was showing mild signs of rejecting the graft. The doctors applied a topical immunosuppressant cream, not approved for use in the United States, and upped Hallam's dosage of anti-inflammatory steroids. The intervention, so far, has worked. Says Dr. Earl Owen, one of the surgeons, ""[We] are already vindicated by the results so far.''
Even if Scott's transplant succeeds, though, its benefits will stop short of miraculous. Doctors told Scott he might hope to recover about 50 percent of a hand's normal function. The day that he can perform fine motor skills, like tying his shoes or buttoning his shirt, ""will not take place,'' says Breidenbach. In patients who have ""replant'' surgery of their own hands, the nerves grow back at a rate of about one millimeter per day, but do not return to full sensation. Patients often cannot feel the difference between, say, a quarter and a nickel. Many complain of chronic stiffness and painful sensitivity to the cold. According to Dr. Diana Carr, a Florida hand surgeon, some patients ""come back and say, "This is not worth the hassle. Take it off'.''
With such high risks and limited benefits, why take the chance? Dr. Vincent Hentz, president of the American Society for Surgery of the Hand, questions whether the doctors should have waited a few years for better anti-rejection drugs. Hand-transplant surgery, says Hentz, ""should be done, and clearly it will be done. Our concern is, Why now? Why use old technology and old drugs? No one is going to die between now and then because we don't do this procedure.''
Breidenbach defends the operation. Before moving forward, his team spent three years consulting and getting approval from ethicists, immunologists and transplant specialists, as well as his hospital's review board. He believes that Scott's operation can yield profound benefits not just for his patient, but for the entire field of reconstructive medicine. These potential benefits, he says, outweigh the risks. ""Let's say we found a [drug protocol] that had minimal complications and was very safe,'' says Breidenbach. ""Then [transplanting] anything's possible. A face or jaw or breast or penis.''
Out of 99 interested candidates, Breidenbach's team conducted intense psychological screening of seven to find the best patient. Scott was promising. Because of his medical training, he was adept with difficult drug protocols. And he had a strong sense of self--important for all transplant patients, who can undergo crises of identity when they realize some of their parts are not their own.
Scott is sober about his prospects. ""This is my opportunity to try and fix what went wrong 13 years ago. And yes, there is a risk involved. If the graft starts overpowering the host--me--and the immunosuppressant therapy becomes detrimental, we can go back and rectify that. We could start by altering my drug therapy. If that's not enough, we'll remove the graft.''
With the help of physical therapists last Friday, Scott flexed the middle joints of his fingers through 40 degrees of motion--ahead of schedule, says Breidenbach. His first biopsy, taken Friday, showed no sign of immune reaction. He may leave the hospital as early as this week, though he'll have to stay in Louisville for the next three months. In the meantime, he said, he calls his two sons, Jeremy, 2, and Ian, 7, in New Jersey every day. ""My youngest one is too young to understand what's really going on,'' he said. ""My oldest thinks this is the coolest thing he's ever seen. To him, Dad's in all the newspapers.''
His wife, Dawn, smiled. ""He thought you were the coolest dad, anyway.''
Scott continued. ""He told me the other day that he can't wait until I get home so I can tickle him with two hands instead of only one, like I've been doing for the seven years of his life.'' For this, Scott has placed his life on the uncertain frontier of experimental medicine. To him, it's worth the risk.
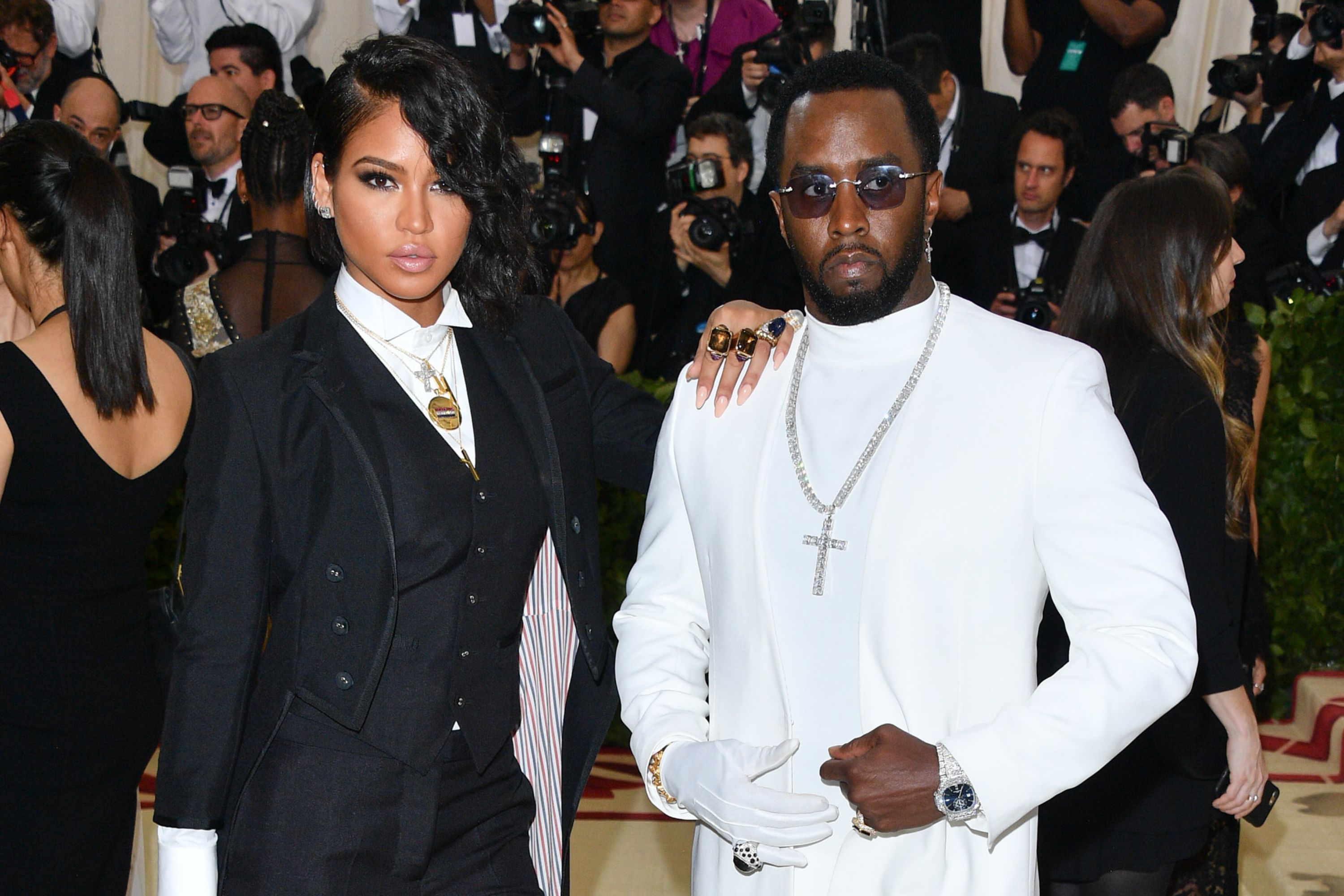
PHOTO (COLOR): Matthew Scott
PHOTOS (COLOR): Body shop: In a macabre twist, the hand attached by Breidenbach (right) came from a convicted murderer who took his own life the day before. Scott expressed only sympathy for the donor's family and thanked him for 'the wonderful gift of my new left hand.'
A SECOND HAND, A SECOND CHANCE It took a 17-member surgical team about 15 hours to complete Matthew Scott's hand transplant, the first in the United States. The operation is extremely complex. Unlike a solid organ transplant--a kidney, for example--a hand reattachment involves multiple tissues: skin, muscle, tendon, bone, nerves and blood vessels. At right, the procedure:
1 Skin and bones: Doctors give Scott general anesthesia. The flow of blood to his lower arm is restricted with a special tourniquet. Curved incisions (diagram A) are made in the forearm and (donor) wrist. Scott's radius and ulna bones are found and lined up with the donor hand's bones. Metal plates secure the bones together (B).
2 Soft tissue: Now the doctors stitch together the arteries (C), tendons (D), nerves and veins (E) on both sides of the arm. This is the longest part of the surgery. Doctors use a very powerful microscope while connecting arteries, nerves and veins; tendons are big enough to attach without magnification.
3 Circulation: After the tissues are attached, the tourniquet is slowly released. The blood begins to flow from Scott's arm into the reattached hand (F). The surgical team watches for the hand to become pink with the return of circulation. They observe the arteries flowing. Then the skin is closed (G) and stitched.
DIAGRAMS: The procedure of Matthew Scott's hand transplant
THE LONG ROAD AHEAD Surgery was only the first step. Scott's body could still reject the hand, and he'll face more hurdles in the future.
Blood clots in arteries and veins are the most serious concern. Doctors monitor for clots by taking a finger temperature--a reading over 89.6 degrees indicates that blood is flowing properly; a temperature below 82.4 degrees indicates a likelihood of cotting. Scott's hand has been at 96.8 degrees since the operation.
Scott's immune system could attack the hand, and that could lead to amputation. Since many types of tissues are attached, there could be a greater chance for rejection. The hand could reject Scott's body, too--this unlikely reversal is called graft-versus-host disease.
Scott will take a cocktail of immunosuppressant drugs to prevent rejection. But they have side effects: metabolic problems, infection and cancer. The metabolic problems include drug-induced diabetes. Scott is already diabetic, and the drugs could aggravate the disease.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.