By all rights, Shari Baker should have said her final goodbyes years ago. In 2005, more than a year after three doctors dismissed a lump under her arm as a harmless cyst, she was diagnosed with stage IV (metastatic) breast cancer, which takes the lives of at least 80 percent of patients within five years; it killed Elizabeth Edwards in 2010. Half of those diagnosed with breast cancer that has spread—in Baker, it had reached her spine—die within 39 months. But the 53-year-old jewelry designer in Scottsdale, Ariz., wasn't ready to die. "I've been a competitive athlete and a body builder, I take care of myself and eat right," she says. "I was going to fight this."
Baker began searching for a clinical trial, and through the International Cancer Advocacy Network (ICAN) found an intriguing possibility: a cancer vaccine. In May 2006, she traveled to the University of Washington. The vaccine was injected into her upper arm; she got five more shots over the next five months. Today, with scans detecting no cancer anywhere, Baker seems to have beaten some extremely stiff odds.
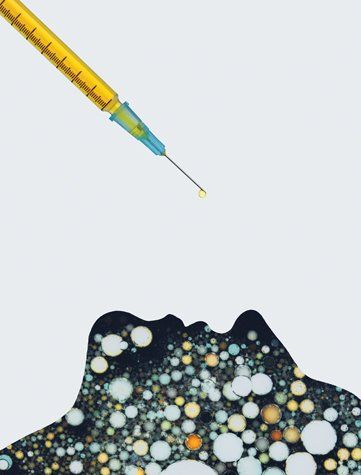
Short of a sci-fi nano-camera to capture what was going on at the cellular level, it's impossible to know exactly what the vaccine did. But based on studies of lab animals and cells in petri dishes, scientists have a pretty good idea. The vaccine contained fragments of a molecule called her2/neu, which, perched on the surface of tumor cells, fuels the growth and proliferation of some breast cancers. Baker's immune system treated the flood of injected her2/neu like an invading army and mounted a counterattack. Cells called CD4, acting like biological Paul Reveres, sounded the alarm, rousing white blood cells called T cells. The body's Minutemen, they invaded Baker's tumor, summoning reinforcements called cytotoxic ("killer") T cells, which destroyed the tumor cells in Baker's breast as well as her spine. Enough of the other 21 women who received the experimental vaccine against metastatic breast cancer are doing so well that its inventor, immunologist Mary ("Nora") Disis of UW, dares to envision a future in which vaccines "control or even eliminate cancer."
After four decades of largely unfulfilled hopes—Dec. 23 marks 40 years since President Nixon declared war on cancer—scientists have hit on a potential cure that few thought possible a few years ago: vaccines. If they succeed, cancer vaccines would revolutionize treatment. They could spell the end of chemotherapy and radiation, which can have horrific side effects, which tumor cells often become resistant to, and which often make so little difference it would be laughable were it not so tragic: last week, for instance, headlines touted two new drugs for metastatic breast cancer even though studies failed to show that they extend survival by a single day. Vaccines could make such "advances" a thing of the past. And they could make cancer as preventable, with a few jabs, as measles.
"Could" is the key word. Cancer vaccines are still being tested. Patients, doctors, and scientists know only too well that seemingly wondrous cancer therapies can flame out. But progress is accelerating. In 2010, the U.S. Food and Drug Administration approved the first-ever tumor vaccine, called Provenge, to treat prostate cancer. Scores of other vaccines are in the pipeline. Over the summer, researchers at the University of Pennsylvania unveiled what they call a cancer "breakthrough 20 years in the making": a vaccine against chronic lymphocytic leukemia (CLL) that has brought about remissions of up to a year and counting—and which its inventors believe can be tweaked to attack lung cancer, ovarian cancer, myeloma, and melanoma. Vaccines against pancreatic and brain cancer are also being tested. "For the first time," says Disis, who has a $7.9 million grant from the Pentagon to develop a preventive vaccine, "clinical trials [of cancer vaccines] are demonstrating anti-tumor efficacy in numbers of patients with cancer, not just one or two unique individuals."
First, some basics. By "cancer vaccine," scientists mean something that will stimulate the immune system to attack malignant cells. The most direct route to that, studies suggest, is by injecting the very same molecules, called antigens, that stud the surface of cancer cells much like Lady Gaga's hats. As with the her2/neu vaccine, that would stimulate T cells to home in on the antigens and encourage the production of killer T cells specific to cells with that antigen. It may seem odd that our bodies would attack our own cells, but by tweaking the antigens, the immune system can be spurred into attacking the tumor. Such a vaccine could be therapeutic, wiping out tumors, or, in theory, preventive, keeping tumors from forming. (Cervical cancer vaccines now on the market are strictly preventive but also unique in that they target cancer-causing viruses; most cancers aren't caused by viruses.)
Harnessing the immune system is completely counter to how cancer is now treated, largely by chemotherapy and radiation. Both can weaken the immune system, which is why some alternative practitioners advise against them. Following that advice can be fatal. But the importance of the immune system in fighting cancer is getting new respect from the nation's leading oncology researchers. It has also inspired a Hail Mary play from a leading advocacy group. Last year, the National Breast Cancer Coalition launched the Artemis Project with the audacious aim of eliminating breast cancer by Jan. 1, 2020. Since the most likely way to accomplish that is through vaccines, says president Fran Visco, NBCC is awarding seed grants for research on, for instance, which antigens make good targets.
NBCC has good timing: research on breast-cancer vaccines is exploding. Last week, the biotechnology firm Antigen Express, Inc., announced that 89 percent of patients who received its her2/neu vaccine were alive after 22 months, compared with 72 percent of nonvaccinated women. The company hopes to get FDA approval for a phase-three trial in 2012. Interestingly, the vaccine seems to help even women who don't qualify for the breast-cancer drug Herceptin because their levels of her2/neu are too low. "We think 75 percent of women with breast cancer could be candidates for the vaccine," says president Eric von Hofe.
Vaccines have the potential to revolutionize cancer treatment because their effects do not stop with existing tumors. Cancer is notorious for its craftiness, changing the biological pathways by which cells proliferate so much that chemotherapies and even targeted molecular therapies soon stop working (that's why even much-hyped drugs such as Avastin increase survival by, at most, a few months). Vaccines could match the cancer cells move for move. In women who receive Disis's vaccine, after T cells destroy breast cancer cells they gobble them up and spit them out. That floods the body with the antigens that adorned the cancer cells, stimulating the immune system to target this second wave of tumor antigens. This spreading immunity creates locked-and-loaded T cells that can destroy tumor cells years after vaccination—the same kind of lifelong immunity that, say, a smallpox vaccine confers.
One final benefit of the cancer vaccine may explain why Shari Baker is alive: T cells never forget. Once the immune system has targeted a threat, be it cancer or smallpox, it keeps a reserve militia ready to attack should that threat return. In principle, that should confer immunity against breast cancer and possibly other cancers as well—forever.
The optimism surrounding cancer vaccines reflects a string of recent discoveries hinting that the immune system can vanquish cancer. Immune activity in and around a tumor—the presence of certain white blood cells—is often a harbinger that a cancer will go into remission and even vanish. A 2006 study, for instance, found that colon cancers that attract killer T cells most strongly are less likely to recur after treatment. Similarly, when early-stage lung cancer cells or some breast cancer cells are studded with T cell–attracting molecules, patients are more likely to dodge metastasis, remain in remission, and live longer. And in liver cancer and ovarian cancer, if the tumor has been invaded by T cells, patients survive longer. There is one final clue to the power of the immune system. "At least 30 percent of tumors found on mammograms would go away even if we did nothing," breast surgeon Susan Love of UCLA told a Project Artemis workshop last spring—a tantalizing hint about the power of the immune system to eliminate cancer.
That raises the obvious question: why does anyone with a working immune system develop cancer, much less die from it? One reason is that tumor cells churn out defensive molecules that repel or destroy T cells. Several experimental therapies are trying to get around that, including an immunotherapy against metastatic melanoma that the FDA approved earlier this year. Called Yervoy, it blocks a molecule known as cytotoxic T lymphocyte antigen (CTLA4), which plays a role in impeding the immune system's ability to fight malignant cells. "That takes the brakes off the immune system and lets it kill the cancers," says tumor immunologist Patrick Hwu of M.D. Anderson Cancer Center, who is developing another melanoma vaccine. But Yervoy, made by Bristol-Myers Squibb and priced at $120,000, extends average survival from 6.5 months to only 10. Doing better, says Hwu, will likely require packing more immune-stimulating molecules into a vaccine.
The National Cancer Institute counts more than 150 kinds of cancer, from the almost-always survivable testicular to the fast-killing pancreatic. Those targeted by experimental vaccines include some of the deadliest, where existing therapies fall tragically short. Last month, for instance, scientists led by NCI tumor immunologist James Gulley announced promising results with a single experimental vaccine against metastatic ovarian and breast cancers. Called PANVAC, it contains genes for two antigens often found on cancer cells, carcinoembryonic antigen (CEA) and mucin1 (MUC1). The 14 ovarian-cancer patients in the study have survived an average of 15 months so far, and the 12 patients with metastatic breast cancer have survived an average of 13.7 months, just slightly better than average. But what stands out for Gulley is a patient whose metastatic breast cancer has "completely disappeared," and who is still alive more than four years after diagnosis. "We see shrinkage of tumors that we've never seen before," says Gulley. Gulley suspects the results might be even better in patients who have not received chemotherapy, which can leave the immune system "beat up."
Vaccines might even tame pancreatic cancer. In March 2010, Bert Williams, 78, heard the worst phrase a doctor can utter: not "you have pancreatic cancer," which Williams had been told in January, but "we didn't get it." The tumor was positioned such that surgically removing it could have proved fatal. Williams thought he was facing a death sentence, but his wife, Gail, found a clinical trial at the Cancer Institute of New Jersey. An oncologist there, Elizabeth Poplin, came to his bedside. We've been looking for you, she said: Williams had yet to receive any cancer treatments that might weaken his immune system and was otherwise healthy. He agreed to receive the experimental vaccine.
The retired advertising executive in Jackson, N.J., received the first injection in March 2010, directly into the tumor. By December, scans detected no tumors anywhere; three of five other patients with inoperable pancreatic cancer are also stable, Poplin and her colleagues reported last month. The best guess is that the vaccine, which floods the body with the tumor antigens CEA and MUC1, stimulated T cells to kill tumor cells tagged with these antigens. "The patients who were vaccinated 13 to 19 months ago are doing well for longer than I am used to," says Poplin. "None have liver or other metastases, which is surprising because pancreatic cancer likes to spread everywhere."
Brain cancer is as deadly as pancreatic cancer, but at least one experimental vaccine is showing promise against glioblastoma multiforme, the most common and aggressive form. It contains bits of the antigen epidermal growth factor receptor variant III, which studs brain cancer cells. In a clinical trial, 18 patients whose tumors had been surgically removed received the vaccine; median survival was 26 months, scientists at Duke University reported in 2010, compared with the usual 14. And in July, Larry Kwak of M.D. Anderson and colleagues reported that in patients given an experimental vaccine against follicular lymphoma, a form of non-Hodgkin's lymphoma, their cancer remained in remission almost twice as long, and counting, as unvaccinated patients. Biovest International plans to seek FDA approval for the vaccine, BiovaxID, in 2012.
Would-be cancer cures have come and gone, and vaccines could fail to live up to our hopes. In many studies, patients like Shari Baker and Bert Williams are exceptions, responding almost miraculously while others derive little or no benefit. The reasons for that difference are under intense study. Some patients are too sick or weak to mount a strong immune response; this is why flu vaccines fail to protect some seniors. Also, immune therapy can take months to work, allowing tumors to grow and metastasize. And if the antigen the vaccine targets is also on healthy cells, killer T cells might go after them, too, causing autoimmune disease.
Despite these challenges, the number of believers in cancer vaccines is growing, and the money is following. Hundreds of clinical trials are recruiting patients (type "cancer and vaccine" into the search box at clinicaltrials.gov). "After many years of failure [with cancer vaccines], we're finally getting it right," says Kwak. Between yesterday and today, another 1,500 people in the U.S. will have died from cancer. There is no time to waste.
Uncommon Knowledge
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
Newsweek is committed to challenging conventional wisdom and finding connections in the search for common ground.
About the writer
To read how Newsweek uses AI as a newsroom tool, Click here.