Of the many ills that can befall the human body, brain damage is one of the most devastating - and confusing. When a person suffers from a traumatic brain injury that leaves him or her in an uncommunicative state, doctors and loved ones face one of medical science's most confounding questions: How do we know when a person is still there? When is a body just a body?
Those question only get more complicated with the startling news that the brains of some patients in a vegetative state appear to recognize familiar faces. The implications are mind-boggling.
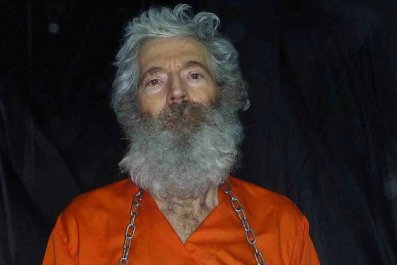
Brain death - when there is zero brain function - is both a medical and legal term, and it is, quite literally, death. But when there is some brain function left, the lines blur rather quickly. A brain-damaged patient may live for months and even years, in limbo: her eyes may open and she may sleep and wake up in what appears to be a normal cycle, but she has no meaningful interactions and shows no awareness of her surroundings - or herself. She is in what the medical community calls a "persistent vegetative state," awake but unaware. It's unlikely that she will ever recover, and if she does, she will probably face severe physical and neurological impairments. Not what most of us call living.
Someone in a vegetative state raises an essential moral and ethical question and an often bitter debate: How much should we do to keep a body on autopilot going? The debate has intensified in recent years, as a few studies have found striking examples of vegetative patients who seem to be able, on some level, to communicate. "With changing paradigms of imaging and other techniques," Dr. Karen Hirsch, a neurologist and neurosurgeon at the Stanford University Medical Center, told Newsweek, "we are learning that maybe some of these people do have some awareness."
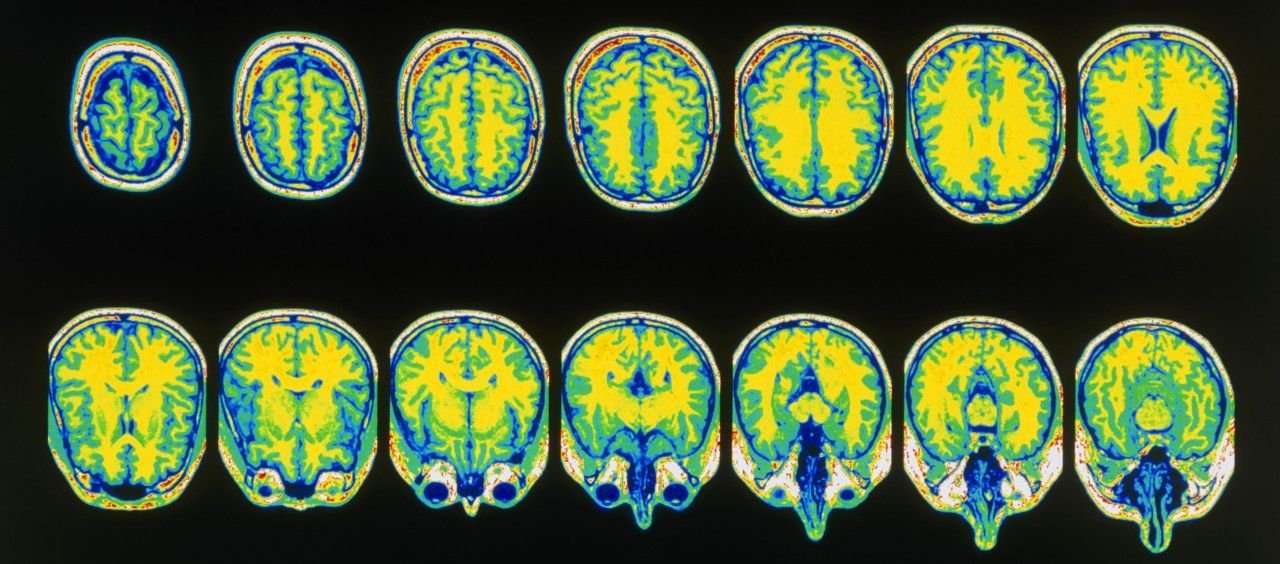
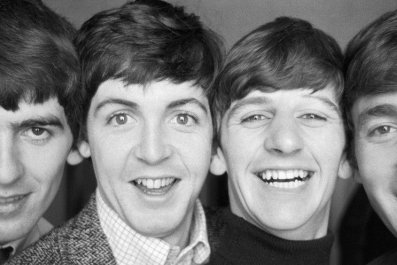
Using functional magnetic resonance imaging (fMRI), researchers working in Tel Aviv looked at the brain activity in both healthy and vegetative subjects. First they showed both groups pictures of strangers, and then pictures of familiar faces. The brain activity patterns of the vegetative patients matched that of the healthy subjects.
That study advances some work released earlier this year: Researchers out of the University of Cambridge said they found that vegetative patients could not only respond to stimulus, but could respond to direct questions with a "yes" or "no" response, and a Western University (Canada) study touted similar results. Both built on a landmark study from a few years earlier, out of Britain and Belgium, in which a handful of patients in vegetative states were "taught" to visualize two specific scenes: one in which they were playing tennis, and another in which they were walking around a familiar place. The researchers claim that one patient was even able to use those two scenes as analogs for "yes" and "no." When asked, for example, "Is your father's name Alexander?" the patient was purportedly able to visualize the scene that corresponded to the correct answer.
There are some large caveats to those studies. In the Cambridge study, "patients" was really "patient," and it took repeating the words "yes" and "no" 5,400 times to get that that patient's brain to develop an "attentiveness" to the words. The Canadian study was the same: Only one of 21 patients studied showed an ability to respond.
These two patients may just be data outliers, cases where the random firings of a primitive brain mimicked the way we think a fully functioning human brain should work. "In all honesty, the majority of patients don't have any underlying function," said Hirsch. "It's just the ones who get published in the literature are the ones that they found something on."
The fMRI technology, however, is accurate, a reliable test to tell doctors which areas of the brain are active. But what "active" actually means also has a little fuzz on it.
"We should be optimistic about these studies but we need to proceed with caution," said Hirsch. "Just because we see areas of the brain light up, that doesn't tell us anything about what the awareness is, what the processing is, or if there is any meaningful sort of context or content for that particularly person."
In other words, it could just be a primitive response to stimulus. Nevertheless, the implications are intriguing. Tracking emotional brain activations can help single out those vegetative patients who may have the best chance at responding to experimental treatments to help them recover. In addition, "Visual, and especially emotional visual stimuli, may also be a way to 'spark' the brain, even in nonresponsive patients with severe brain injuries," Dr. Haggai Sharon, a researcher at Tel Aviv University's Functional Brain Center, and the study's lead author, told Newsweek.
Further, this line of research could potentially solve one of the most difficult problems of neurological critical care, one very much tied up in lines drawn between living and not: determining when to continue providing medical care and when to let go. If we could effectively communicate with the patient herself, perhaps we could simply ask whether or not she wants to go on living. However, "we are still a long way from communicating with patients in such a way," Sharon said.
In the meanwhile, we can't rely on science to make those decisions. "It's important to take the taboo and stigma out of talking about brain injury and death and dying, and to bring it into the forefront of the conversations we have with loved ones," said Hirsch.
What these studies also show is that ethics and morals are personal, and the parameters of what defines "life" are as ill-defined in science as they are in philosophy and art.